Faça Download do PDF Completo – Cirurgia catarata e buraco macular
Henry B. Smith, MA, MBBS, MRCOphth, Nelson A. Sabrosa, MD, PhD, Niall Patton, MD, FRCOphth, Robert E. MacLaren, DPhil, FRCOphth
We describe a technique for combined fluid–gas exchange and phacoemulsification 2 weeks after macular hole surgery to achieve rapid visual rehabilitation. The procedure uses a standard cataract set and requires minimal vitreoretinal expertise. We encountered no significant complications and obtained long-term outcomes comparable to those with conventional management.
Financial Disclosure: No author has a financial or proprietary interest in any material or method mentioned.
J Cataract Refract Surg 2011; 37:229–234 Q 2011 ASCRS and ESCRS
There is currently a debate about whether to posture patients face-down after vitrectomy and gas for macular hole treatment.1 A requirement for posturing may deter some patients, particularly those with musculoskeletal problems, from having surgery. Other sequelae such as deep vein thrombosis and ulnar nerve palsies are also reported.2 Advocates of nonprone posturing cite pilot studies showing macular hole closure rates of 88% to 92% without face-down posturing.3–5 Those in favor of posturing find support in a recent prospective randomized clinical trial of 150 eyes6 that showed a higher closure rate in patients randomized to prone posturing than in those randomized to nonprone posturing (97% versus 88%, PZ .027). However, in that study the overall results were skewed by a marked difference in one subgroup of patients who had larger holes (500 m m to 800 m m) treated with hexafluoroethane gas. This makes it difficult to extrapolate the conclusions of that study to macular hole surgery using perfluoropropane (C3 F8 ) gas, which is more widely used in other studies and is longer-acting, providing a larger bubble in the immediate postoperative period. Although the posturing debate is unresolved, it seems reasonable to assume that the greater surface area in the immediate postoperative period will ensure that long-acting gases such as C3 F8 will cover macular holes more effectively, despite varying orientations of the eye. Such gases would, therefore, be preferable for nonprone posturing, particularly for larger holes.
As most patients develop or already have cataract, another topic of debate is whether to perform phacoemulsification at the same time as macular hole surgery or as a separate procedure.3 In addition to patient convenience, advantages of a combined procedure include the opportunity for a more complete anterior vitrectomy and the introduction of a slightly larger bubble. Having gas in the eye may, however, cause problems with lens displacement and optic capture in up to 9% of cases.7 Small biometry errors have also been reported due to a myopic shift following combined phacovitrectomy cases (possibly due to anterior lens displacement).8 In many centers, service issues and specialist expertise determine the way the surgery is performed; frequently as 2 sequential procedures, with vitrectomy and gas followed by cataract extraction at a later date. In the latter case, cataract extraction is usually performed once the gas has reabsorbed and the hole is confirmed to be closed several months after the vitrectomy.
Another issue of debate relates to the type of gas used. Long-acting gases such as C3 F8 have the advantage of providing a larger bubble in the immediate postoperative period, but they remain in the eye for many months. This can be a significant cause of visual morbidity in patients with poor vision in the fellow eye. The inferior field defect associated with the residual bubble at later stages is a risk factor for falls when going downstairs in elderly patients.9 Long-acting intraocular gas is also inconvenient for those who have to drive a vehicle or travel by air in the early postoperative period. Observations from early optical coherence tomography (OCT) studies show that the macular hole achieves anatomical closure within the first 24 to 72 hours after surgery.10,11 Hence, it is likely that the presence of gas in the eye for weeks or months after surgery has little or no therapeutic benefit.
Taking these factors into consideration, we sought to optimize surgery in selected patients who required rapid visual rehabilitation by removing the gas 2 weeks after surgery. By moving up the time of the subsequent cataract surgery, it was possible to combine the 2 procedures relatively easily, without requiring extra hospital visits. Long-acting gas could also be used without reservation, which may be helpful in patients who are not prone postured or those with larger holes.
In our center, patients routinely have macular hole surgery comprising vitrectomy, internal limiting membrane peeling, and 14% to 16% C3 F8 intraocular gas, followed later by phacoemulsification cataract surgery, as required. In a few selected individuals, as an alternative to using silicone oil, we moved up the cataract surgery and combined it with removal of gas at 2 weeks to achieve rapid visual rehabilitation. This paper describes the technique and presents the results of a retrospective review of complication rates and outcome in the first patients to have the procedure.
SURGICAL TECHNIQUE
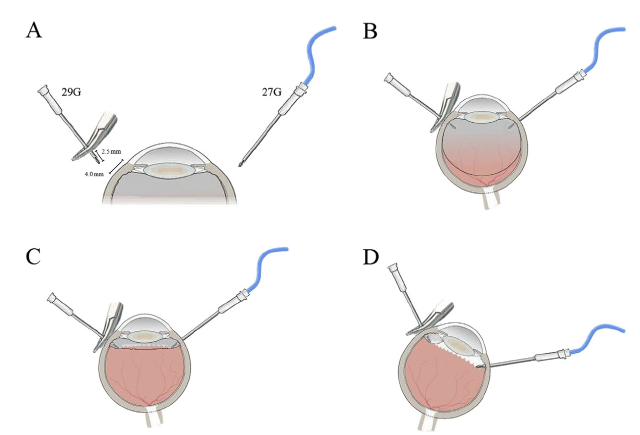
The process of gas removal and phacoemulsification is achieved using equipment readily available during conventional cataract surgery. The first step is to perform a fluid–gas exchange. To maintain positive pressure in the eye, the irrigation line from the phacoemulsification system is used. The line is temporarily disconnected from the phaco handpiece and attached to a 27-gauge half-inch needle. This needle is passed obliquely through the conjunctiva and sclera 4.0 mm posterior to the limbus in the inferotemporal quadrant of the eye, avoiding the original infusion port. When the needle tip is seen through the pupil, the bottle height is raised to 2 meters and a balanced salt solution infusion commenced. Free flow is confirmed by visualizing the Purkinje image of the fluid level through the lens, seen as regular wave-like golden splashes. The rate of flow slows and eventually ceases as the IOP equilibrates with the infusion pressure over a period of 15 to 20 seconds.
When the infusion pressure is stabilized, the next stage is to allow controlled escape of gas. This is achieved by inserting a 29-gauge half-inch needle obliquely through the conjunctiva and sclera 4.0 mm posterior to the limbus in the superonasal quadrant (Figure 1, A). To obtain an optimal internal depth in the eye, the 29-gauge needle is clamped 2.5 mm from the tip with a pair of curved artery forceps. This also provides a secure grip for the needle while the other hand holds the infusion line. At 2.5 mm into the conjunctival surface, the needle tip sits within the vitreous cavity but beyond the vitreous base (Figure 1, B). The infusion is then started, displacing gas through the 29-gauge needle (Figure 1, C). Tilting the eye allows maximum egress of gas and also guards against lens touch. Sustained release of gas can be confirmed indirectly by observing a trickling of the infusion fluid, which causes a rippling of the golden fluid level reflex seen through the pupil. Toward the end of the gas removal, the fluid level rises to meet the posterior surface of the lens and the red reflex is restored. At this point, the eye is rotated inferotemporally with the 29-gauge needle uppermost, facilitating removal of the residual pocket of gas (Figure 1, D).
When the fluid–gas exchange appears complete, the 29-gauge gas removal needle is withdrawn from the eye; a few more bubbles of gas commonly escape. The eye is then rotated back into the neutral position and the IOP checked manually before the infusion is stopped and the 27-gauge needle connected to it is withdrawn. A small cotton tip or swap is used to massage the conjunctiva after the needle is removed to improve wound integrity.
With the red reflex restored, conventional phacoemulsification through a clear corneal incision can be performed. During the irrigation/aspiration phase, a small residual gas bubble may roll under the posterior capsule if the anterior chamber is allowed to shallow. This causes anterior bulging of the posterior capsule and loss of the red reflex, but by maintaining the infusion pressure and tilting the eye inferiorly the bubble can easily be displaced back behind the zonules (Video, available at https://jcrsjournal.org).
Patients are reviewed the following day to check IOP and assess hole closure. Repeat OCT scans and final Snellen visual acuity assessments are performed in the clinic approximately 2 to 3 months later.
Results
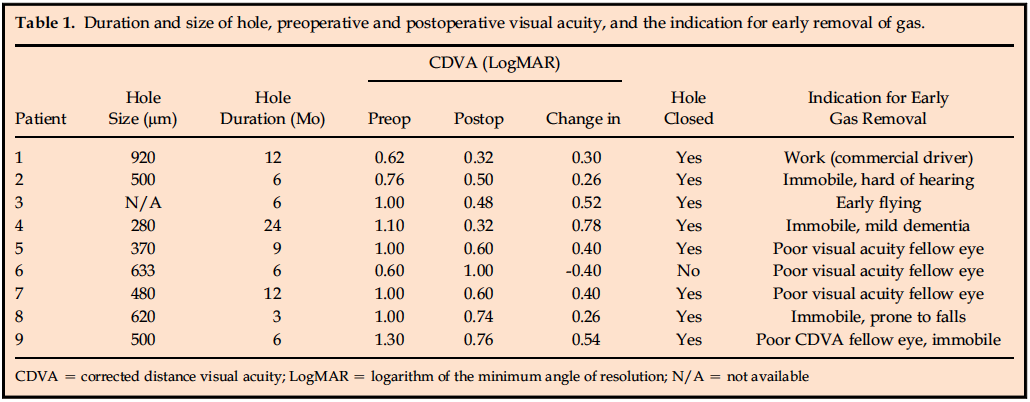
Patients suitable for early removal of gas were identified prior to the initial surgery and consented
to the combined procedure. The mean age of the 6 women and 3 men was 71 years (range 52 to 81 years). One patient (Table 1 , patient 9) was pseudophakic, but all others had at least some degree of cataract prior to macular hole surgery. The pseudophakic patient had hand movement vision in his fellow eye due to chronic panuveitis (ankylosing spondylitis) and secondary glaucomatous optic neuropathy. His macular hole had initially been treated by phacovitrectomy, internal limiting membrane peel, and 20% sulphur hexafluoride (SF6 ) with facedown posturing, but this subsequently proved impossible due to his spondylosis. The hole failed to close, and his visual acuity remained poor at 1.30 logMAR. Repeat surgery was performed 3 months later using 14% C3 F8 , but the patient found the poor vision in both eyes extremely debilitating and the intraocular pressure (IOP) was difficult to control. After 2 weeks, the decision was made to remove the gas using the technique described, although because the patient was pseudophakic, the phacoemulsification step was not required. The other 8 patients had a planned combined procedure with the indications for early removal of gas listed in Table 1 .
The mean hole size, measured by OCT before the initial surgery, was 538 m m (range 280 to 920 m m). Biometry was also obtained at this stage. Macular hole surgery was performed using standard 20-gauge instrumentation and included peeling of the internal limiting membrane with enhanced trypan blue and the use of 14% C3 F8 gas. Patients were asked to lie face down overnight immediately after surgery to prevent pupil block during the period of maximum gas expansion but were otherwise advised to avoid looking up.
They were also asked to minimize their physical activity as excess head movement might cause fluid in the posterior segment to wash over the hole and break the surface tension. The patients were reviewed on the first postoperative day, and all had near total gas fills
(conventional face-down posturing would have been advocated if the gas fill had been incomplete).
Two weeks after the initial surgery, the patients were readmitted for the second procedure to remove the gas and perform cataract extraction with intraocular lens implantation. Prior to surgery, all patients were examined in the supine position by indirect ophthalmoscopy to exclude obviously open holes. At this stage, the gas fill was about 30% and a view of the macula was possible in all but 1 patient who had a significant gas cataract (Table 1, patient 6). If the hole had remained open, a further period of prone posturing or a gas top-up combined with cataract extraction might have been advised. However, no open holes were identified in the 8 maculas visualized at this stage.
Anatomical closurewas achieved in 8 of the 9 cases as assessed by OCT at 2 months after surgery. In the 1 patient in whom the hole failed to close (Table 1, patient 6), a repeat gas exchange and 1 week of prone posturing was undertaken. However, the hole remained open after this repeat procedure and the patient’s vision did not improve. Overall, the procedure was associated with a significant improvement in visual acuity across the cohort, with a mean preoperative logMAR of 0.93 improving to 0.59 (PZ.013).
The procedure itself was initially awkward because of difficulties removing a sufficient amount of gas. The problem was solved by clamping the gas outlet needle 2.5 mm from the tip, keeping it just within the eye and allowing gas to escape down to a very small bubble. On one occasion, extra fluid had to be injected through the pars plana to correct mild ocular hypotony, which might have compromised the wound architecture of the subsequent corneal incision. There were no other surgical complications, although a reduced pupil size and gas cataract precluded accurate assessment of hole closure by indirect ophthalmoscopy in all cases. Optical coherence tomography was performed at a 2-month follow-up visit to confirm the status of the macula; in the 8 cases in which closure was achieved, the holes remained closed during a variable followup period of 3 to 9 months.
The gauge of needles was chosen to be optimal for controlled gas exchange while leaving self-sealing scleral wounds. For the infusion, 27-gauge was the smallest bore that allowed sufficient fluid to enter the eye through the infusion line with the bottle height at 2 meters. For gas removal, 29-gauge was the smallest that allowed free flow of gas. An insulin syringe was unsuitable because any fluid trapped within the body of the syringe generated too much resistance to allow gas to escape. Placing the 29-gauge gas port superonasally positioned the tip of the needle in the most superior dependent position when the eye was rotated, facilitating removal of the rising bubble as it became smaller (Table 1).
DISCUSSION
We describe a technique of phacoemulsification in gasfilled eyes, which is occasionally indicated in selected cases following macular hole surgery. We have audited the outcome of this procedure in 9 patients and show that the success of hole closure is comparable to that in standard surgery in which the gas is left to reabsorb spontaneously over several months. Combining early gas removal with cataract surgery can be performed safely and without an additional procedure. This may be a particularly useful technique for patients who have poor vision in the fellow eye or who need to travel by air in the immediate postoperative period. The technique described uses a standard cataract set with the phacoemulsification infusion line used to perform the fluid–gas exchange, making the costs of the additional procedure minimal.
In our series, at least 4 patients would not have had the procedure had early gas removal not been available. One was dependent on driving for his income and could not afford to take 3 months off work (Table 1, patient 1), while 3 had such poor vision in their fellow eye that they would have been incapacitated by the loss of navigational vision in the eye with the macular hole (Table 1, patients 5, 6, and 9). In similar cases, or in cases in which posturing is not possible, the use of silicone oil has been shown to be effective in hole closure.12 Silicone, however, is associated with additional surgical complications and the removal procedure is arguably more complex than removing gas, as described here. In cases in which holes fail to close using gas tamponade, the use of heavy silicone oil has also been advocated, and a recent study has shown it to be effective at closing 11 of 12 holes that failed primary surgery with SF6.13 It is, however, possible that the success of hole closure is not due to the oil itself but simply reflects a more sustained tamponade of the hole, which might be achieved in nonprone patients with a very longacting gas. Unfortunately, many patients who cannot perform prone posturing also have mobility problems and these are arguably the worst candidates for the prolonged scotoma associated with long-acting gases such as C3F8. In these situations, a mobile inferior field defect is likely to impair visual coordination, particularly when going downstairs.
In our case series, early removal of gas led to a hole closure rate comparable to that which would be expected following conventional macular hole surgery. A prospective randomized controlled trial to prove this, however, may be impractical for 2 principal reasons. First, a noninferiority calculation predicts that 446 subjects would be required to provide adequate power to demonstrate a statistically significant difference of 5% or less between this technique and conventional surgery (assuming a success rate of 90% for the latter). Second, as this technique would be reserved for patients in whom there was a clear advantage to early visual rehabilitation, many may choose not to proceed if randomized to a conventional arm.
A potential criticismof separating macular hole surgery from gas removal and phacoemulsification by only 2 weeks is that it would subject the blood–retinal barrier to a double insult in a relatively short period of time. This could promote inflammatory processes such as cystoid macular edema. However, singlestep phacovitrectomy with gas is likely to cause more inflammation than standard cataract surgery, as shown by a higher rate of posterior synechiae formation, possibly due to the displacement of inflammatory proteins into the anterior segment.14 We are advocating this procedure as an alternative to phacovitrectomy, or to short-acting or mediumacting gases with later cataract surgery, but specifically for patients who need long-acting gases and who require rapid visual rehabilitation.
The debate about posturing after macular hole surgery and the type of gas to use continues, but we propose a third way: nonprone posturing with long-acting gas, which is removed 2 weeks later in combination with cataract surgery. In our series, this achieved rapid visual rehabilitation without complications. Given the ability to remove the gas, even longer-acting preparations such as perfluorobutane (C4F10) (with a half-life more than 3 times that of C3F8) could be considered.15 Macular hole surgery with nonexpansible C4F10 and subsequent removal by the technique we have described may represent a viable alternative to silicone oil in selected cases.
REFERENCES
1. Dhawahir-Scala FE, Maino A, Saha K, Mokashi AA, McLauchlan R, Charles S. To posture or not to posture after macular hole surgery. Retina 2008; 28:60–65
2. Holekamp NM, Meredith TA, Landers MB, Snyder WB, Thompson JT, Berman AG, Williams S. Ulnar neuropathy as a complication of macular hole surgery. Arch Ophthalmol 1999; 117:1607–1610. Available at: https://archopht.amaassn. org/cgi/reprint/117/12/1607.pdf. Accessed October 18, 2010
3. Simcock PR, Scalia S. Phacovitrectomy without prone posturing for full thickness macular holes. Br J Ophthalmol 2001; 85:1316– 1319. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC1723751/pdf/v085p01316.pdf. Accessed October 18, 2010
4. Tranos PG, Peter NM, Nath R, Singh M, Dimitrakos S, Charteris D, Kon C. Macular hole surgery without prone posturing. Eye 2007; 21:802–806
5. Rubinstein A, Any A, Patel CK. Vitrectomy without postoperative posturing for idiopathic macular holes. Clin Exp Ophthalmol 2007; 35:458–461
6. Guillaubey A, Malvitte L, LaFontaine PO, Jay N, Hubert I, Bron A, Berrod JP, Creuzot-Garcher C. Comparison of face-down and seated position after idiopathic macular hole surgery: a randomized clinical trial. Am J Ophthalmol 2008; 146:128–134
7. Rahman R, Rosen PH. Pupillary capture after combined management of cataract and vitreoretinal pathology. J Cataract Refract Surg 2002; 28:1607–1612
8. Falkner-Radler CI, Benesch T, Binder S. Accuracy of preoperative biometry in vitrectomy combined with cataract surgery for patients with epiretinal membranes and macular holes; results of a prospective controlled clinical trial. J Cataract Refract Surg 2008; 34:1754–1760
9. Haymes SA, LeBlanc RP, Nicolela MT, Chiasson LA, Chauhan BC. Risk of falls and motor vehicle collisions in glaucoma. Invest Ophthalmol Vis Sci 2007; 48:1149–1155. Available at: https://www.iovs.org/cgi/reprint/48/3/1149. Accessed October 18, 2010
10. Sato H, Kawasaki R, Yamashita H. Observations of idiopathic full-thickness macular hole closure in early postoperative period as evaluated by optical coherence tomography. Am J Ophthalmol 2003; 136:185–187
11. Satchi K, Patel CK. Posterior chamber compartments demonstrated by optical coherence tomography, in silicone-filled eyes, following macular hole surgery. Clin Exp Ophthalmol 2005; 33:619–622
12. Goldbaum MH, McCuen BW 2nd, Hanneken AM, Burgess SK, Chen HH. Silicone oil tamponade to seal macular holes without position restrictions. Ophthalmology 1998; 105:2140–2147
13. Lappas A, Heinrich Foerster AM, Kirchhof B. Use of heavy silicone oil (Densiron-68) in the treatment of persistent macular holes. Acta Ophthalmol (Oxf) 2009; 87: 866–870
14. Li W, Sun G,WuR, Wang X, Xu M, Sun C. Longterm results after phacovitrectomy and foldable intraocular lens implantation. Acta Ophthalmol (Oxf) 2009; 87:896–900
15. Lincoff A, Lincoff H, Iwamoto T, Jacobiec F, Kreissig I. Perfluoron- butane; a gas for a maximum duration retinal tamponade. Arch Ophthalmol 1983; 101:460–462. Available at: https://archopht. ama-assn.org/cgi/reprint/101/3/460. Accessed October 18, 2010
